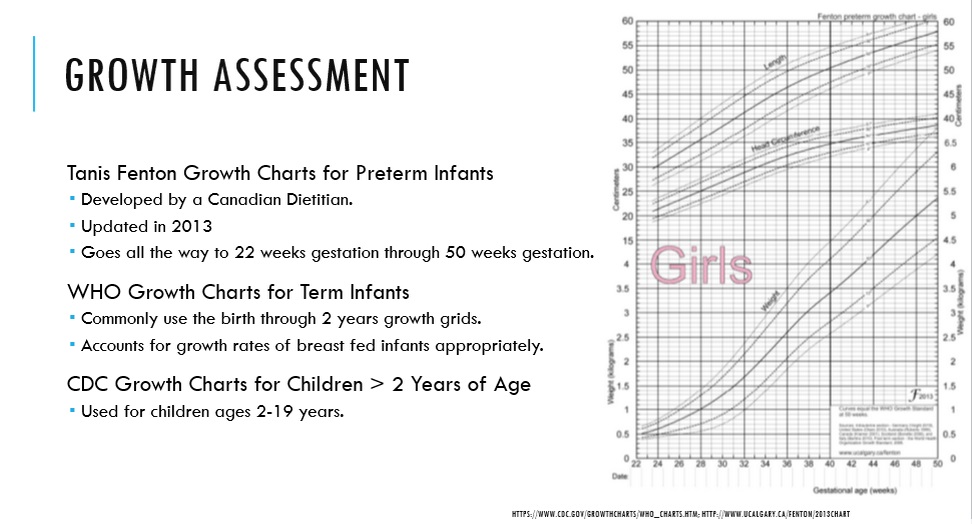
I wanted to do a quick write up about donating breastmilk to the Indiana Milk Bank. I was able to drop off some of my extra milk to the Milk Bank and I was very excited and wanted to share about that experience. I was able to go through the approval process to become a donor. Then I went ahead and donated 687oz of frozen breastmilk. My mother had this milk in her deep freezer and she helped me drop it off at Columbus Regional Hospital. I was so excited to be able to give some of my milk to the Milk Bank to sell to hospital to use for preterm babies.
If you are a breastfeeding mother and have extra breastmilk, you should consider becoming a breastmilk donor. Check out my first post about this - CLICK HERE.
I also donated some breastmilk to a random stranger on Facebook .... gasp! I know right? I was torn about it. But here is why I did it ... I had some breastmilk that had been in a refrigerator/freezer for > 6months and I wasn't able to donate it to the Milk Bank. There standards can < 6months in a refrigerator/freezer. This was milk that I didn't need and I wanted it to go to someone that could use it. There was a lady on a Swap Group I belong to on Facebook who was needing donor breastmilk for her little one and she hadn't been able to find anyone with extra milk. I really felt like I could and should help her. I felt like I wanted her to get good, safe milk and I let her know that I was an approved donor through the Milk Bank. I was able to give her over 200 oz of breastmilk. Normally I am not a fan of just giving away your breastmilk to a stranger, but I felt like if you think about it and do what you feel comfortable with that can be the write call.
I also wanted to touch on breast pumps. I have had several people ask me about my breast pump. I went ahead and purchased a Medela Symphony. This pump is a hospital grade pump and it is what you would use while in the hospital or if your baby was in the NICU. This is a great pump, but is very expensive to purchase on your own. Insurance won't purchase it for you. I was very torn about what type of pump to purchase. I really liked Medela, but there are so many different options and I kept hearing such mixed messages about all of them. I was really stressing about it and that is when my husband suggested we look online for a used Symphony. We found one on Ebay that was ~$600 and it has ~75 hours on the machine. This was a great deal when retail value is ~$1000. I knew that this pump would work well and I wouldn't stress about it. If I had rented the same pump through the hospital it is $60 a month and over the course of 12 months that costs $720. So I knew that I would get my money worth out of that pump if I purchased it on my own. I just wanted to share that story with you, because I don't think people realize that you can purchase a used Symphony pump. Now, please be smart about it when you shop on Ebay. But if you really want that hospital grade pump there are ways to obtain one for less than the retail price of $1000.
If you are looking at getting a breastmilk pump through your insurance .... do your research, look online and talk to your friends. Try to figure out what pumps have good reviews and evaluate what would work for you. This is a big decision and you need to make sure that you are making the best choice for you and your little one.